Hyperplastic polyp in gastric heterotopia - Not everything is as it seems!
Jéssica de Lima Chaves, Ana Clara Vasconcelos, Richard Azevedo, Pedro Bastos, Diogo Libânio, Catarina Brandão
Serviço de Gastrenterologia Instituto Português de Oncologia do Porto
DESCRIPTION
We present a case of a 59-year-old man referred to our center with a suspected esophageal neoplasm detected during a screening upper gastrointestinal endoscopy (UGIE) with previous negative biopsies. A follow-up UGIE revealed an elevated, polypoid, erythematous lesion between the 18 and 20cm from the incisors, with underlying salmon-colored mucosae (figure 1a and 1b).
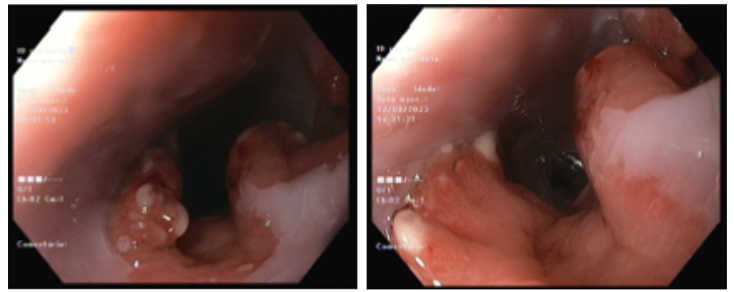
Figure 1a and 1b
The lesion covered two-thirds of the esophageal circumference, without causing luminal narrowing and presented no clear disruption of the mucosal pattern (figures 2a and 2b). These findings were suggestive of hyperplastic/granulation tissue in gastric heterotopia, and several biopsies were taken.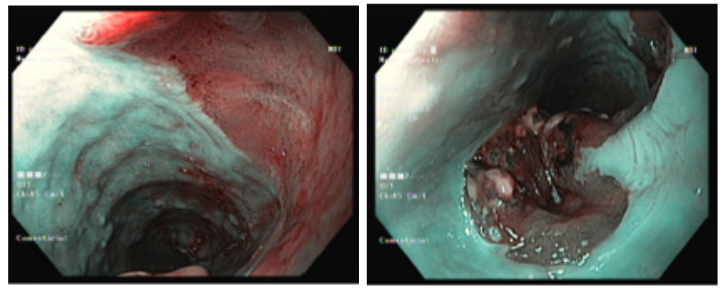
Figure 2a and 2b
A previously planned staging endoscopic ultrasound was performed showing thickening of the mucosal layer in the proximal esophagus, with no further involvement of other layers (figure 3) and without suspicious adenopathies. Histopathology identified esophageal mucosa lined with stratified squamous epithelium, as well as gastric-type columnar epithelium with areas of erosion, granulation tissue, and moderate mixed inflammatory infiltrate. These findings were compatible with the diagnosis of a hyperplastic polyp in gastric heterotopia in the proximal esophagus.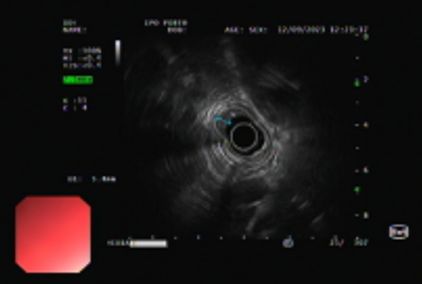
Figure 3
DISCUSSION
First described over 200 years ago by Schmidt, gastric heterotopia is a common finding in UGIE, being estimated to be present in 0.1-10% of all patients undergoing diagnostic UGIE.1,2
Gastric heterotopia is usually detected as a flat salmon-colored area in asymptomatic individuals. However, due to potential acid production and its frequent location in the proximal esophagus (being also prone to mechanical stress), several symptoms—such as globus, cough, sore throat, and hoarseness—have been described. Rarely, complications such as esophageal strictures or webs have been reported, and a few cases of adenocarcinoma have been documented in the literature.1,2,3
In addition to standard medical treatment with proton pump inhibitors (even though with scarce evidence), endoscopic treatment options, including ablation or resection techniques, may be offered to symptomatic patients or those with dysplastic lesions.1,2
In our case, the patient was asymptomatic, and UGIE was performed for unrelated reasons. Endoscopic, ultrasound, and histopathological findings were combined, leading to the diagnosis of a hyperplastic polyp in gastric heterotopia. Given the low risk of dysplastic progression, the absence of symptoms, and the risk for adverse events, the lesion was not resected, and the patient was advised to undergo endoscopic surveillance.
REFERENCES
1. Rusu R, Ishaq S, Wong T, Dunn JM. Cervical inlet patch: new insights into diagnosis and endoscopic therapy. Frontline Gastroenterol. 2018 Jul;9(3):214-220
2. Phrathep DD, Anthony S, Healey KD, Ward I, Herman M. Symptoms of Chronic Dysphagia Secondary to Multiple Cervical Inlet Patches and Esophageal Stricture. Cureus. 2023 Jan 6;15(1):e33459
3. Patel A, Ajumobi AB. Esophageal Stricture: An Uncommon Complication of Cervical Inlet Patch. J Investig Med High Impact Case Rep. 2023 Jan-Dec;11:23247096231201024


