The danger of manipulating colonic lesions before endoscopic resection
Inês Pita, Iolanda Ribeiro, Mafalda Sousa, Samuel Costa, Manuel Correia, Rute Cerqueira, Ricardo Veloso
Serviço de Gastrenterologia – Unidade Local de Saúde Entre Douro e Vouga
DESCRIPTION
A 66-year-old male was referred to the hospital for removal of a 25-mm Paris 0-IIa non-granular lesion in the sigmoid colon. Four months later, at the therapeutic colonoscopy, the lesion had a depressed and irregular center (JNET type 2b) and an underlying submucosal tattoo was noted (figure 1A and 1B). The procedure was done after oral bowel preparation and using CO2 insufflation. The lesion was elevated with submucosal injection of saline and methylene blue, with suboptimal elevation in the centre (figure 1C).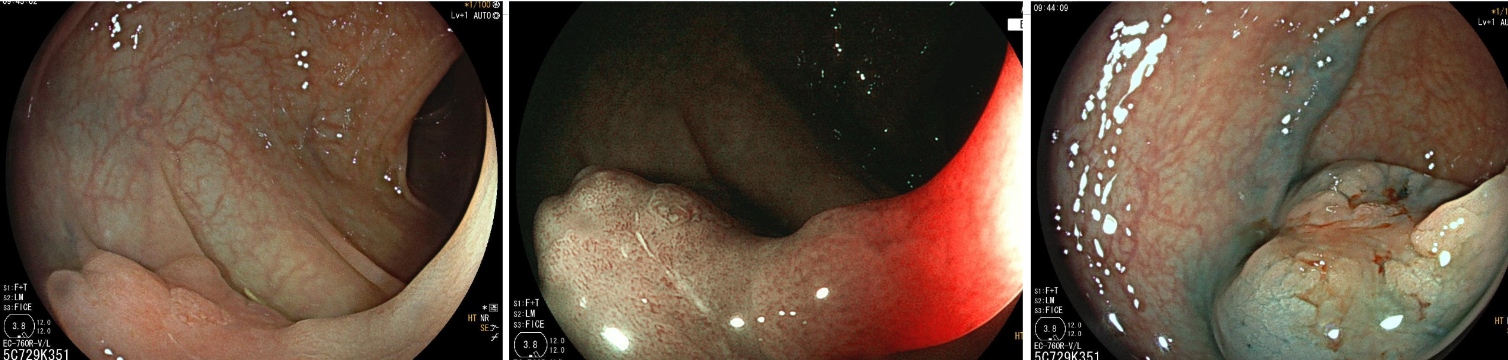
Figure 1A Figure 1B Figure 1C
The lesion was grasped with a 20 mm oval braided snare and resected en bloc. After resection, a free perforation was noted (Sydney type IV defect) and a corresponding target sign was seen in the resected specimen (figures 2A and 2B). A 10 mm over-the-scope clip (OTSC) was mounted and deployed around the defect, using gentle aspiration to guide the defect margins into the cap. After deployment, the defect was inspected and was apparently completely contained inside the clip’s claws (figure 2C).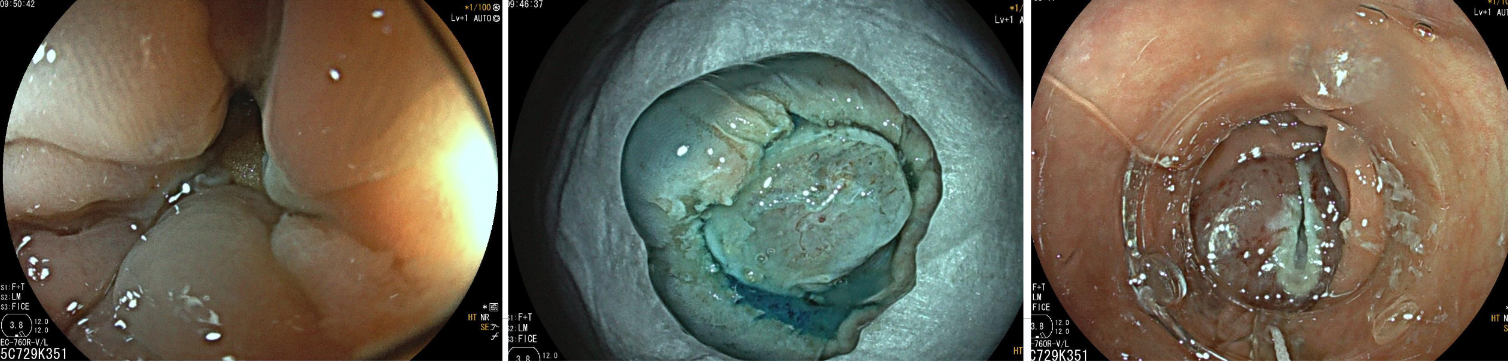
Figure 2A Figure 2B Figure 3C
The patient was admitted for surveillance and started antibiotics. He was discharged after 5 days, without further complications. The pathology report revealed a tubular adenoma with low-grade dysplasia.
DISCUSSION
In this case, it is possible that the underlying tattoo resulted in submucosal fibrosis, which prevented adequate lesion lifting. The resulting perforation, although small, was felt to be difficult to adequately close with through-the-scope clips due to defect shape and location. During OTSC deployment, vigorous aspiration pulled extra-luminal fat into the cap, which hindered visualization of the defect margins and risked capturing extra-colonic structures into the clip. Adequate defect closure was achieved with gentle aspiration, to permit adequate cap positioning.
This case highlights the dangers of manipulating lesions before their resection: either taking biopsies, lesion injection without resection, or tattooing under a lesion, have been associated with a risk of submucosal fibrosis, which may hinder subsequent resection attempts. [1, 2, 3]. For these reasons, whenever lesions are referred for endoscopic resection, biopsies or “trial” injection should be avoided, and if the lesion is tattooed, it should be placed at least 5 cm distally from the lesion. When there is manipulation of the lesion, prompt referral and scheduling for definitive resection should be prioritized, because delays in definitive resection of previously manipulated polyps are associated with an increased incidence of fibrosis with time and associated inferior outcomes [4].
REFERENCES
1. Emmanuel A. et al. Outcomes of endoscopic resection of large colorectal lesions subjected to prior failed resection or substantial manipulation. Int J Colorectal Dis 2019; 34(6):1033-1041.
2. Kim HG et al. Effect of prior biopsy sampling, tattoo placement, and snare sampling on endoscopic resection of large nonpedunculated colorectal lesions. Gastrointest Endosc 2015 Jan;81(1):204-213.
3. Friedland S et al. Endoscopic management of nonlifting colon polyps. Diagn Ther Endosc. 2013;2013:412936. Epub 2013 May 14.
4. Ayoub F et al. Delays in definitive endoscopic resection of previously manipulated colorectal polyps as a risk factor for inferior resection outcomes. Gastrointest Endosc. 2024 Jul;100(1):109-115.


