When electricity fails: Iatrogenic perforation during choledochoduodenostomy for biliary drainage of malignant biliary obstruction
Francisca Côrte-Real1, Nuno Nunes1, Ana Rita Silva1, Diogo Bernardo Moura1, Ana Catarina Rego1, Maria Antónia Duarte1
1Hospital do Divino Espírito Santo de Ponta Delgada, EPER
DESCRIPTION
An 88-year-old man was admitted with jaundice, choluria and pruritus. He had been diagnosed with diabetes mellitus type 2 six months earlier. Laboratory analysis showed cytocholestasis (TGO 166 U/L, TGP 159 U/L, alkaline phosphatase 402 U/L and GGT 395 U/L), with hyperbilirrubinaemia - total bilirubin 8.08 mg/dL and direct bilirrubin 6.93 mg/dL, with normal amylasemia and C-reactive protein levels.
An abdominal ultrasound showed a 24x18 mm hypoechoic mass, in the pancreatic head/uncinate process, suspicious for atypia. There was dilation of the pancreatic duct (5 mm) and common bile duct (12 mm) - double duct sign, as well as moderate dilation of the intra- hepatic bile ducts.
The patient refused any treatment. However, he accepted an endoscopic approach to jaundice palliation. A retrograde cholangiopancreatography (ERCP) was attempted. The biliary cannulation of the common bile duct (CBD) was not possible, even after pre-cut papillotomy. The endoscopic ultrasound (EUS) showed a short and tight stenosis of the distal CBD and the proximal CBD was dilated (13 mm).
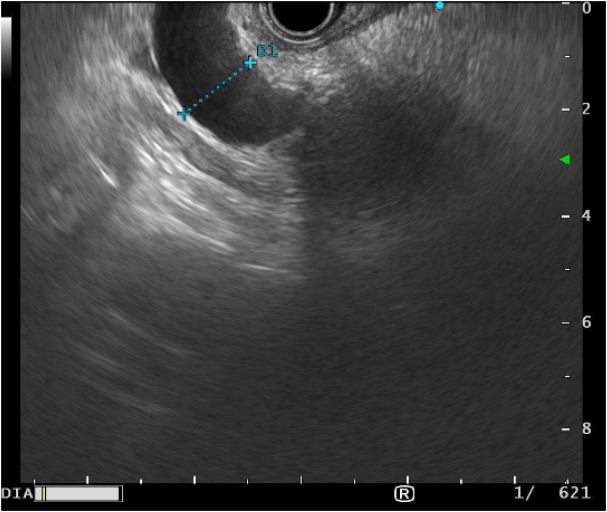
Figure 1. Hypoechoic nodule in the head of the pancreas that causes a short and tight stenosis, with dilation of the common bile duct (13 mm).
A choledochoduodenostomy with lumen-apposing metal stent (LAMS), with a Hot AXIOSTM (8x6 mm) was performed. During the procedure, the delivery system did not work because the source of electrocautery was not connected, and a mechanical perforation happened. After ensuring the correct functioning of the system, a successful choledochoduodenostomy was performed. There was an immediate drainage of bile stasis under great pressure.
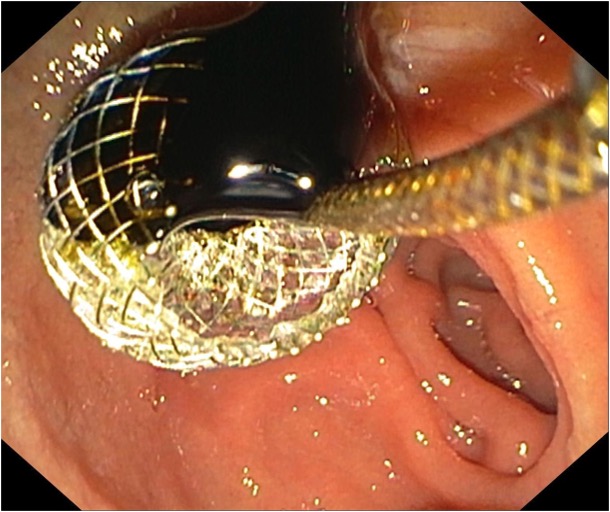
Figure 2. Choledochoduodenostomy with LAMS.
We checked for the possibility of a small hole related to the first puncture, which was found. It measured 4 mm, located 5 mm away from the LAMS. The perforation was successfully closed with 3 through-the-scope (TTS) clips.
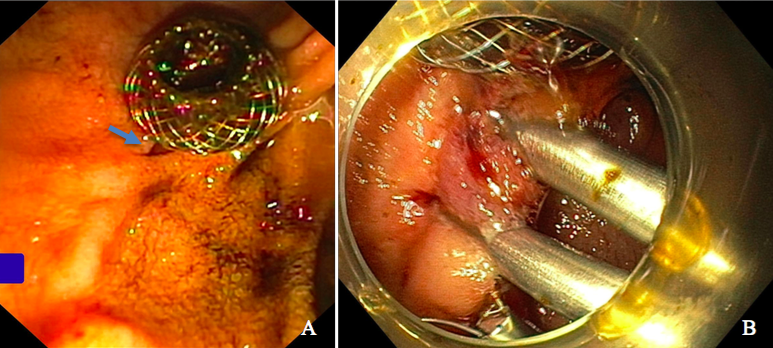
Figure 3. Perforation from first choledochoduodenostomy (A) and its closure, with 3 through-the-scope clips (B).
The patient remained clinically stable and stayed one day at the hospital for observation and antibiotherapy. Jaundice resolved, with no need for further procedures during the follow-up of four months.
DISCUSSION:
In the event of malignant biliary obstruction, the endoscopic placement of a metallic biliary stent improves quality of life and decrease morbidity and mortality.1,2 Malignant extrahepatic biliary obstruction decompression should preferably be performed by endoscopic retrograde cholangiopancreatography (ERCP), when compared to surgery or percutaneous drainage.3 When ERCP is not possible, endoscopic ultrasound (EUS) should be considered, since it allows the lumen apposing metal stent (LAMS) placement in a single-step procedure.1,2 This is a fast alternative technique to ERCP, with high success rates and a low risk of complications.2 With this case, we aim to highlight the importance of early identification of complications associated with the endoscopic technique and their immediate resolution, thus providing other complications, namely biliary peritonitis ant pneumoperitoneum.4
REFERENCES:
1. Torres, K. et. al. Choledochoduodenostomy with LAMS (Hot-Axios type) for malignant obstructive jaundice — An increasingly used technique. Rev Esp Enferm Dig.2022 Sep;114(9):558-559.
2. Ducreux, M. et al. Cancer of the Pancreas: ESMO Clinical Practice Guidelines. Ann Oncol (2015) 26 (suppl 5): v56-v68.
3. van der Merwe, SW. et al. Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2022; 54: 185–205.
4. Altonbary, AY. et al. Endoscopic ultrasound guided biliary drainage: a multicenter retrospective experience of a technique slowly gaining acceptance in Egypt. Ther Adv Gastrointest Endosc. 2019 Jan-Dec; 12: 2631774519889456.


