Esophageal endoscopic submucosal dissection: its feasibility is possible in locations with difficult access
Sara Archer1, Tiago Pereira Guedes1, Ana Teresa Ferreira1, Sofia Ponte1, André Ruge2, Ana Sadio1, Ricardo Marcos-Pinto1, Sílvia Barrias1, Isabel Pedroto1, Ricardo Küttner Magalhães1
1 Unidade Local de Saúde de Santo António
2 Unidade local de Saúde de Leiria
DESCRIPTION
A 57-year-old male was referred due to an esophageal lesion with high-grade dysplasia. Endoscopic re-evaluation using white-light, narrow-band imaging, and lugol chromoendoscopy revealed a 55mm, Paris 0-IIa lesion, involving about 80% of the luminal circumference, with the cranial border located at the upperesophageal sphincter area (Figure 1).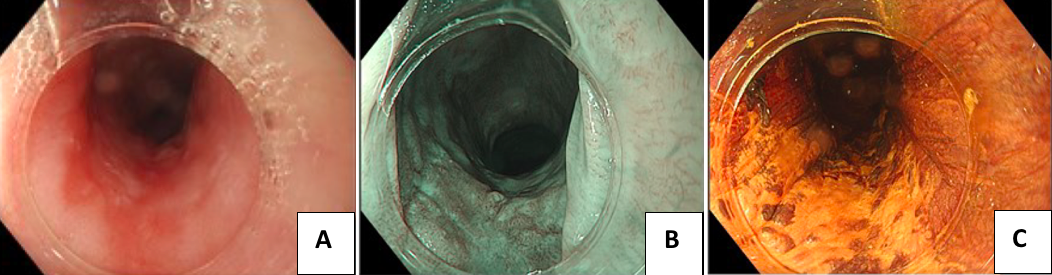
Figure 1. Endoscopic evaluation using white-light (A), narrow-band imaging (B), and lugol chromoendoscopy (C).
Endoscopic submucosal dissection (ESD) was performed. Proximal and distal circumferential incisions were made using a Gold knife, Micro Tech-T 1,5mm. Next, a tunnel was accomplished. The additional use of the clip-with-line technique allowed traction of the specimen, enabling en bloc resection of a 62mm in length specimen (Figure 2). Lastly, triamcinolone was injected into the residual submucosal layer of the ulcer bed, which involved 90% of the luminal circumference. The patient was discharged under oral prednisolone. Histological examination revealed an R0 resection of a m2 squamous cell carcinoma, well-differentiated, without lymphovascular invasion.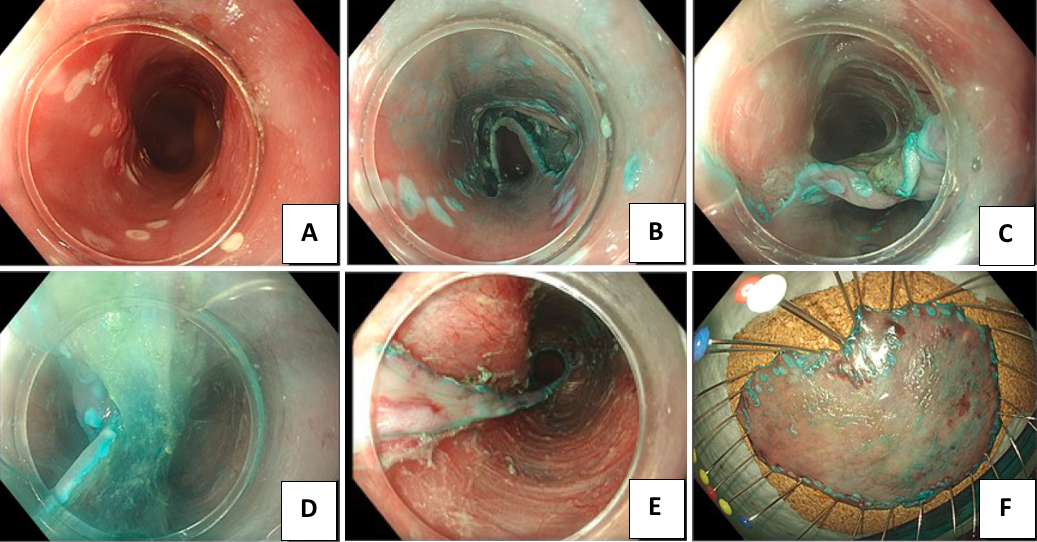
Figure 2. Steps of the procedure: (A) Marking; (B) Incision; (C) Submucosal dissection using tunneling technique; (D) Additional use of the clip-with-line technique allowed traction of the specimen; (E) Post-resection ulcer; (F) Resected specimen.
Two months after the procedure, he presented with an esophageal stenosis, requiring successive dilations and the placement of a fully covered self-expanding metallic stent.
DISCUSSION:
Performing ESD near the pharyngoesophageal junction is particularly demanding. Apart from the inherent complexity associated with esophageal ESD due to its circular configuration, decreased thickness of the muscle wall, and the influence of both respiratory and cardiac movements, this location imposes a significant limitation to the endoscope maneuverability. We present a successful esophageal ESD performed on a lesion located at the level of the upper esophageal sphincter, by combining tunneling and clip-with-line techniques. This case raises awareness not only about the challenge of this technically demanding but feasible procedure, but also on the important role of high-definition endoscopy, electronic chromoscopy and conventional chromoscopy with lugol for the identification and characterization of suspicious lesions of squamous cell carcinoma.


